
Little is known about the exact etiology of Schizoaffective Disorder, although researchers believe that,the risk for schizoaffective disorder may be increased among individuals who have a first-degree relative with schizophrenia, biploar disorder, or schizoaffective disorder. There is some clinical evidence to suggest that Schizoid, Schizotypal, Borderline, or Paranoid Personality Disorders may be present before the onset of Schizoaffective Disorder.
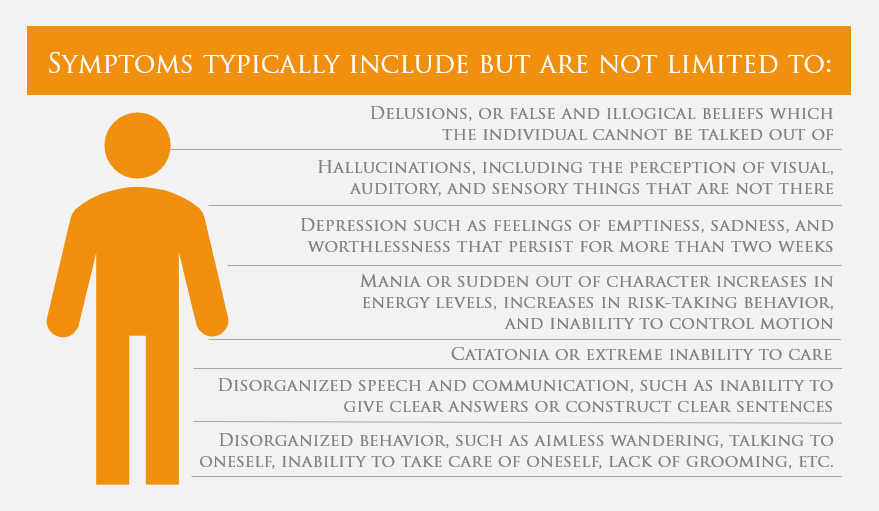
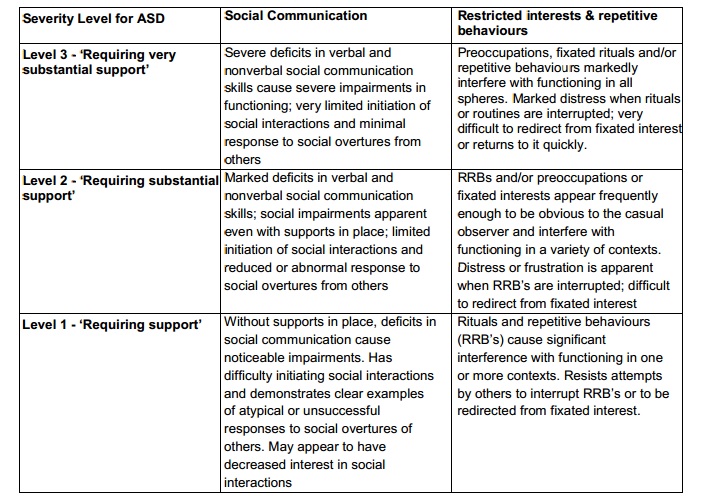
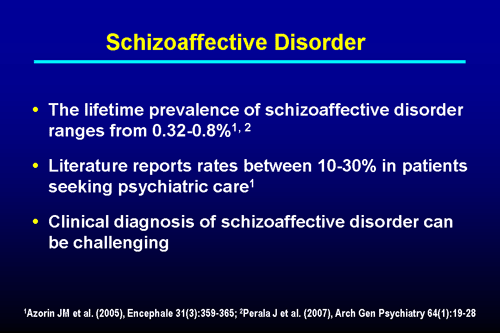
Individuals with Schizoaffective Disorder may also experience difficulties with alcohol- or substance-related disorders. Factors associated with poor prognosis include lack of precipitating factors, insidious onset, poor premorbid history, presence of Depressive Type rather than Bipolar Type, presence of negative/deficit symptoms, earlier onset, unremitting course, and having a relative with schizophrenia. Residual symptoms, negative/deficit symptoms, and deficits in insight tend to be less severe in Schizoaffective Disorder than in schizophrenia. On average, the prognosis for Schizoaffective Disorder is better than that for schizophrenia but worse than the prognosis for Mood Disorders. Evidence suggests that Bipolar Type is more likely to occur in younger adults, while Depressive Type is more likely to occur in older adults. The typical age of onset is during early adulthood. Schizoaffective disorder appears to be about one-third as common as schizophrenia and the life-time prevalence is estimated at 0.3%. Schizoaffective Disorder is seen more often in women than in men, accounted for by women’s increased rates of Schizoaffective Disorder, Depressive Type. They may be lonely and have restricted social lives, relying heavily on support from their families. Individuals with Schizoaffective Disorder may demonstrate poor occupational functioning as well as impaired self-care abilities. (2) Depressive Type is used to denote cases in which only Major Depressive Episodes have occurred. (1) Bipolar Type is used to denote cases in which a Manic Episode has occurred Depressive Episodes may also have been present but are not required for this specifier. Schizoaffective Disorder is categorized into two subtypes. In addition, symptoms that meet diagnostic criteria for a Mood Episode must be present for a substantial portion of the illness. More specifically, a diagnosis of Schizoaffective Disorder requires an uninterrupted period of illness, at least one month in duration, in which a Major Depressive or Manic Episode is concurrent with symptoms that meet Criterion A for schizophrenia - which requires two or more of the following symptoms: delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, and negative/deficit symptoms (e.g., poverty of speech, a volition, affective flattening).Ī diagnosis of Schizoaffective Disorder requires that during the period of illness, there be at least two weeks in which psychotic symptoms are present in the absence of prominent mood symptoms, in order to ascertain that the schizophrenic symptoms are not a direct result of the Mood Disorder. Schizoaffective Disorder is a diagnosis from the chapter on Schizophrenia Spectrum and Other Psychotic Disorder that is characterized by symptoms of both schizophrenia and a mood episode. Transcript of DSM-5 EPPP Lecture Video: Schizoaffective Disorder
#Schizoaffective disorder dsm 5 series
To watch earlier lectures in this series, or register for our webinar series on DSM-5 and the EPPP, click HERE. This lecture series aims to equip those preparing for the EPPP with everything you need to know about the impact DSM-5 will be having on the EPPP. The video below is the section for Schizoaffective Disorder from Part 7 of TSM’s lecture series on DSM-5 and the EPPP, followed by a transcript.


 0 kommentar(er)
0 kommentar(er)
